Cardiogenic Pulmonary Edema: Understanding a Life-Threatening Condition
Introduction
Cardiogenic pulmonary edema (CPE) is a serious medical condition characterized by the accumulation of fluid in the lungs due to heart dysfunction. This condition can lead to acute respiratory failure and, if not treated promptly, can be fatal. Understanding CPE is crucial for both healthcare professionals and patients, as early recognition and intervention can significantly improve outcomes.
What is Cardiogenic Pulmonary Edema?
Cardiogenic pulmonary edema occurs when the heart is unable to pump blood effectively, leading to increased pressure in the pulmonary veins. This elevated pressure causes fluid to leak from the blood vessels into the lung tissues and alveoli, impairing gas exchange and leading to symptoms such as shortness of breath and coughing up pink, frothy sputum. CPE is often associated with conditions such as heart failure, myocardial infarction, and severe hypertension.
Historical Background
The understanding of cardiogenic pulmonary edema has evolved over centuries. Initially thought to be a direct result of lung disease, it was later recognized that heart dysfunction plays a critical role. The term “pulmonary edema” was first used in the early 19th century, but it wasn’t until the mid-20th century that the link between cardiac conditions and pulmonary edema was firmly established. Advances in medical imaging and echocardiography have further enhanced our ability to diagnose and manage this condition.
Anatomy and Pathophysiology
The lungs consist of alveoli surrounded by capillaries, where gas exchange occurs. In a healthy state, fluid balance between these two structures is maintained by Starling forces. However, in CPE, increased left atrial pressure leads to elevated pulmonary capillary pressure, resulting in fluid transudation into the alveoli. This process disrupts normal gas exchange and can lead to hypoxemia.Key anatomical components involved include:
- Alveolar-capillary membrane: The barrier between air in the alveoli and blood in the capillaries.
- Lymphatic system: Responsible for draining excess fluid; its dysfunction can exacerbate edema.
Causes
Several factors contribute to the development of cardiogenic pulmonary edema:
- Acute decompensated heart failure: The most common cause.
- Myocardial infarction: Damage to heart muscle impairs pumping ability.
- Valvular heart disease: Conditions like mitral regurgitation increase left atrial pressure.
- Severe hypertension: High blood pressure can lead to increased workload on the heart.
- Fluid overload: Such as from renal failure or excessive intravenous fluids.
Symptoms and Clinical Presentation
Patients with cardiogenic pulmonary edema typically present with:
- Dyspnea: Shortness of breath that may worsen when lying down.
- Tachypnea: Rapid breathing.
- Coughing: Often producing pink, frothy sputum.
- Cyanosis: Bluish discoloration of lips or extremities due to low oxygen levels.
- Anxiety: Often due to difficulty breathing.
Physical examination may reveal crackles in lung auscultation and signs of fluid overload such as peripheral edema.
Diagnosis
Diagnosing CPE involves a combination of clinical evaluation and diagnostic tests:
- History and physical examination: Assessing symptoms and risk factors.
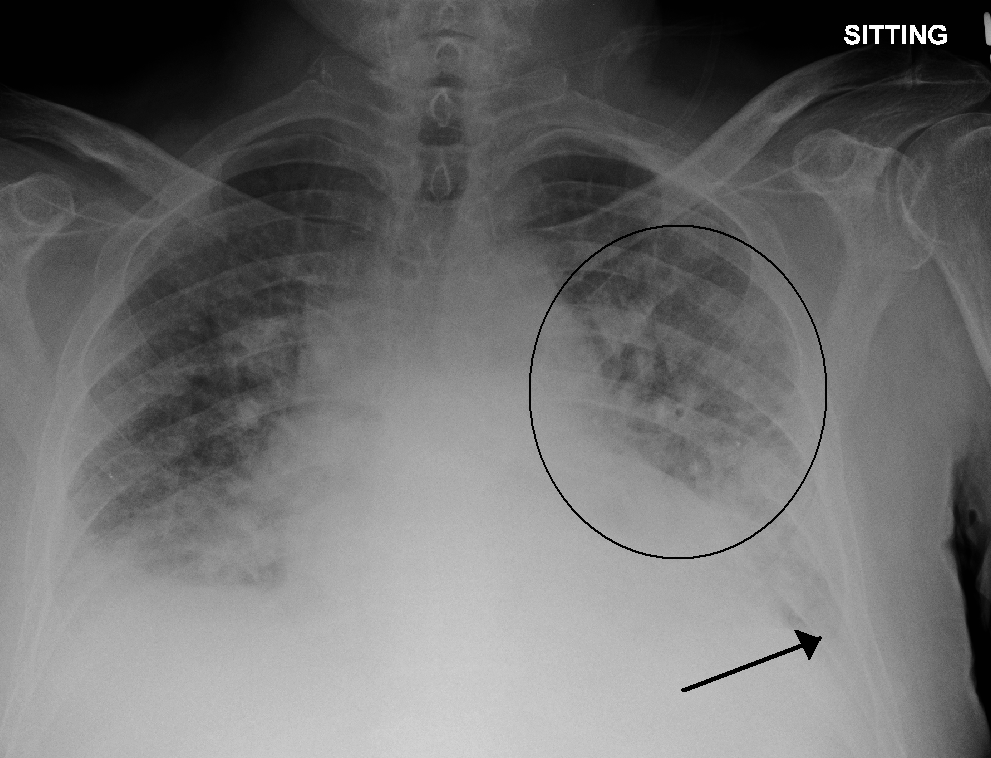
- Imaging studies: Chest X-rays can show fluid in the lungs; echocardiograms assess heart function.
- Laboratory tests: Blood tests including BNP (B-type natriuretic peptide) can indicate heart failure.
Early diagnosis is critical for effective management.
Treatment Options
Management of cardiogenic pulmonary edema focuses on addressing both symptoms and underlying causes:
- Diuretics: To reduce fluid overload.
- Oxygen therapy: To improve oxygenation.
- Vasodilators: To decrease cardiac workload by reducing systemic vascular resistance.
- Inotropes: Medications that strengthen heart contractions may be necessary in severe cases.
- Non-invasive ventilation: Such as CPAP or BiPAP, can assist breathing during acute episodes.
Prognosis and Recovery
The prognosis for patients with cardiogenic pulmonary edema largely depends on the underlying cause and timeliness of treatment. Mortality rates can be high without prompt intervention, with studies indicating an in-hospital death rate of 15–20%. Long-term survival varies widely based on individual health conditions but typically shows a significant decline over years if underlying issues are not managed effectively.
Living with Cardiogenic Pulmonary Edema
For individuals diagnosed with CPE or at risk for developing it:
- Lifestyle modifications: Adopting a heart-healthy diet, engaging in regular physical activity, and managing stress are vital.
- Medication adherence: Consistent use of prescribed medications can help manage heart failure symptoms and prevent episodes of pulmonary edema.
- Regular follow-ups: Ongoing medical evaluations are essential for monitoring heart function and adjusting treatment plans as needed.
Research and Future Directions
Ongoing research aims to better understand the pathophysiology of cardiogenic pulmonary edema and explore new treatment modalities. Studies are focusing on:
- Genetic predispositions: Identifying genetic markers that may increase susceptibility.
- Innovative therapies: Investigating novel pharmacological agents that could enhance diuresis or improve cardiac contractility without adverse effects.
Future advancements may lead to more personalized treatment approaches that improve outcomes for patients suffering from this complex condition.
Conclusion
Cardiogenic pulmonary edema is a critical medical condition requiring immediate attention. Understanding its causes, symptoms, diagnosis, and treatment options is essential for effective management. With appropriate care and lifestyle adjustments, individuals can improve their quality of life while managing this serious health issue.
Disclaimer
This article is intended for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for diagnosis and treatment options tailored to your specific condition.
