Cardiorenal Syndrome: Understanding the Interplay Between Heart and Kidney Health
Introduction
Cardiorenal syndrome (CRS) is a complex condition that involves the interplay between the heart and kidneys, where dysfunction in one organ adversely affects the other. This syndrome poses significant challenges in clinical management and has been associated with poor outcomes in patients with heart failure and chronic kidney disease. Understanding cardiorenal syndrome is essential for healthcare providers and patients alike, as early recognition and appropriate intervention can improve prognosis. This article explores the various facets of cardiorenal syndrome, including its definition, historical context, anatomy, causes, symptoms, diagnosis, treatment options, prognosis, and future research directions.
What is Cardiorenal Syndrome?
Cardiorenal syndrome refers to a spectrum of disorders characterized by the simultaneous dysfunction of the heart and kidneys. It is classified into five types based on the primary organ affected:
- Type 1: Acute cardiorenal syndrome—acute worsening of cardiac function leading to acute kidney injury.
- Type 2: Chronic cardiorenal syndrome—chronic heart failure leading to progressive chronic kidney disease.
- Type 3: Acute renocardiac syndrome—acute kidney injury leading to acute cardiac dysfunction.
- Type 4: Chronic renocardiac syndrome—chronic kidney disease leading to cardiac dysfunction.
- Type 5: Secondary cardiorenal syndrome—systemic conditions affecting both organs (e.g., sepsis).
The interdependence of these organs means that dysfunction in one can exacerbate issues in the other, creating a vicious cycle that complicates treatment.
Historical Background
The recognition of the relationship between cardiac and renal dysfunction dates back several decades. Early studies primarily focused on heart failure and its impact on renal function, but it wasn’t until the late 20th century that researchers began to systematically study cardiorenal syndrome as a distinct clinical entity. The term “cardiorenal syndrome” was formally introduced in medical literature in the early 2000s, highlighting the need for a comprehensive understanding of how these two vital organs interact.As research progressed, it became evident that both acute and chronic conditions could lead to significant morbidity and mortality when cardiac and renal functions were compromised simultaneously. This led to increased awareness among healthcare professionals about the importance of managing both organ systems concurrently.
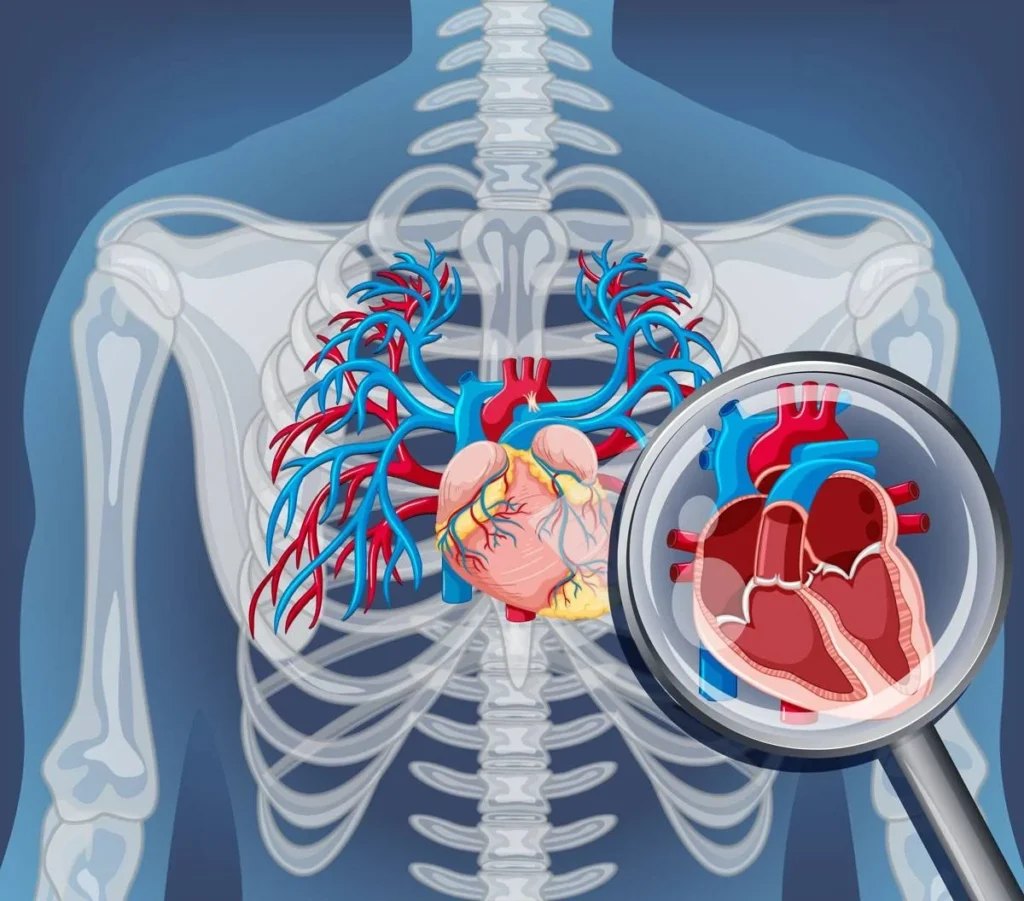
Anatomy and Pathophysiology
The heart and kidneys are intricately linked through various physiological mechanisms:
- Cardiac Output: The heart pumps blood to the kidneys for filtration. Reduced cardiac output due to heart failure can lead to decreased renal perfusion, triggering compensatory mechanisms such as activation of the renin-angiotensin-aldosterone system (RAAS).
- Fluid Overload: Heart failure can lead to fluid retention, which increases venous pressure and further compromises kidney function.
- Neurohormonal Activation: In response to decreased blood flow, neurohormonal systems become activated, exacerbating fluid retention and hypertension.
This complex interplay results in a cycle where heart dysfunction leads to kidney impairment, which in turn worsens heart function—a phenomenon that underscores the importance of integrated management strategies.
Causes
Several factors contribute to the development of cardiorenal syndrome:
- Heart Failure: The most common cause, where impaired cardiac function leads to renal hypoperfusion.
- Chronic Kidney Disease: Reduced kidney function can cause fluid overload and increased cardiovascular strain.
- Acute Kidney Injury: Conditions like dehydration or sepsis can lead to sudden renal impairment affecting cardiac performance.
- Systemic Diseases: Conditions such as diabetes mellitus or hypertension can predispose individuals to both heart and kidney dysfunction.
Understanding these underlying causes is crucial for effective prevention and management strategies.
Symptoms and Clinical Presentation
Symptoms of cardiorenal syndrome can vary based on which organ is primarily affected but often include:
- Shortness of Breath: Due to fluid overload from heart failure.
- Fatigue: Resulting from decreased cardiac output.
- Swelling: Peripheral edema due to fluid retention.
- Decreased Urine Output: Indicative of impaired kidney function.
- Chest Pain or Discomfort: May occur due to underlying cardiac issues.
Patients may present with a combination of these symptoms, making accurate diagnosis challenging.
Diagnosis
Diagnosing cardiorenal syndrome involves a thorough clinical evaluation:
- Medical History and Physical Examination: Identifying risk factors such as history of heart disease or kidney problems.
- Laboratory Tests:
- Complete blood count
- Comprehensive metabolic panel
- Urine studies (e.g., protein-to-creatinine ratio)
- Brain natriuretic peptide (BNP) levels
- Troponin tests for myocardial injury
- Imaging Studies:
- Echocardiography to assess cardiac function
- Renal ultrasound to evaluate kidney size and structure
- Hemodynamic Monitoring: In severe cases, invasive monitoring may be required to assess blood flow dynamics.
Early diagnosis is essential for timely intervention.
Treatment Options
Management of cardiorenal syndrome focuses on addressing both cardiac and renal dysfunction:
- Diuretics:
- Used to manage fluid overload by promoting urine production.
- Common agents include furosemide (Lasix) and torsemide (Demadex).
- Vasodilators:
- Help reduce systemic vascular resistance, improving blood flow.
- Medications like nitroglycerin may be employed.
- Inotropes:
- Drugs such as dobutamine may be used in acute settings to enhance cardiac contractility.
- Renal Replacement Therapy (RRT):
- In severe cases of acute kidney injury or fluid overload, dialysis may be necessary.
- Neurohormonal Modulation:
- Angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) help manage hypertension while providing renal protection.
- Extracorporeal Therapies:
- Techniques like ultrafiltration can effectively remove excess fluid without causing significant hemodynamic instability.
A multidisciplinary approach involving cardiologists, nephrologists, and primary care providers is essential for optimal management.
Prognosis and Recovery
The prognosis for patients with cardiorenal syndrome varies widely based on several factors:
- Severity of Dysfunction: Patients with advanced heart failure or chronic kidney disease typically have poorer outcomes.
- Timeliness of Treatment: Early recognition and intervention significantly improve prognosis.
- Underlying Causes: Addressing comorbid conditions such as diabetes or hypertension can enhance recovery prospects.
While full recovery may not always be achievable, effective management can improve quality of life and reduce complications.
Living with Cardiorenal Syndrome
Living with cardiorenal syndrome requires ongoing management strategies:
- Regular Monitoring: Frequent follow-ups with healthcare providers are crucial for assessing organ function.
- Lifestyle Modifications:
- Adopting a heart-healthy diet low in sodium and saturated fats
- Engaging in regular physical activity tailored to individual capabilities
- Avoiding smoking and excessive alcohol consumption
- Medication Adherence: Consistent use of prescribed medications is vital for managing symptoms effectively.
Support from family members or participation in support groups can provide emotional resilience during challenging times.
Research and Future Directions
Ongoing research aims to better understand cardiorenal syndrome’s pathophysiology and explore new treatment modalities:
- Investigating biomarkers that could predict worsening renal or cardiac function more accurately.
- Exploring novel pharmacological agents that target both cardiac output enhancement and renal protection simultaneously.
- Studying lifestyle interventions that could mitigate the progression of both heart failure and chronic kidney disease.
Future studies will likely focus on personalized medicine approaches that consider individual patient profiles for more effective management strategies.
Conclusion
Cardiorenal syndrome represents a complex interplay between cardiac and renal health that poses significant challenges for patients and healthcare providers alike. Understanding its causes, symptoms, diagnostic methods, treatment options, and ongoing research efforts is crucial for effective management. With timely intervention and a comprehensive approach, individuals affected by this condition can achieve better health outcomes and improved quality of life.
Disclaimer
This article is intended for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for diagnosis and treatment options tailored to your specific condition.
