Cerebrovascular Disease: Understanding a Leading Cause of Disability and Death
Introduction
Cerebrovascular disease encompasses a range of disorders that affect the blood vessels supplying the brain. These conditions can lead to serious complications, including strokes, transient ischemic attacks (TIAs), and other vascular problems that can significantly impact quality of life. With cerebrovascular disease being one of the leading causes of death and disability worldwide, understanding its causes, symptoms, diagnosis, and treatment options is crucial for prevention and management.
What is Cerebrovascular Disease?
Cerebrovascular disease refers to a group of medical conditions that affect blood flow to the brain. It includes disorders such as ischemic strokes, hemorrhagic strokes, TIAs, and vascular malformations. When blood flow is interrupted or reduced due to blockages or ruptures in blood vessels, brain cells can become damaged or die from lack of oxygen and nutrients. This can lead to varying degrees of neurological impairment.
Historical Background
The recognition and understanding of cerebrovascular disease have evolved significantly over the years. Early medical texts described strokes as “apoplexy,” with little understanding of their underlying mechanisms. In the 19th century, advancements in medical imaging and research began to shed light on the causes and types of cerebrovascular events. The development of techniques such as CT and MRI scans has revolutionized diagnosis, allowing for more effective treatment strategies.
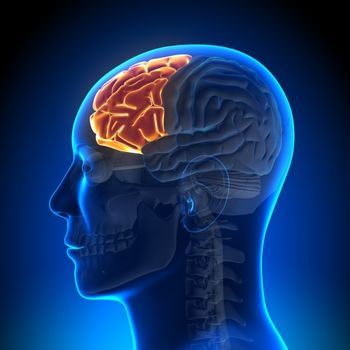
Anatomy and Pathophysiology
The brain relies on a complex network of arteries and veins to ensure adequate blood supply. Key anatomical structures involved in cerebrovascular disease include:
- Carotid Arteries: Major arteries that supply blood to the front part of the brain.
- Vertebral Arteries: Supply blood to the back part of the brain.
- Cerebral Veins: Drain deoxygenated blood from the brain back to the heart.
Pathophysiologically, cerebrovascular disease can result from various processes:
- Ischemia: Reduced blood flow due to blockages (thrombosis or embolism) can lead to ischemic strokes.
- Hemorrhage: Rupture of blood vessels can cause bleeding in or around the brain (hemorrhagic stroke).
- Atherosclerosis: The buildup of fatty deposits in arteries can narrow them, increasing the risk of clots.
Understanding these mechanisms is essential for recognizing risk factors and implementing preventive measures.
Causes
Cerebrovascular disease can arise from several risk factors:
- Hypertension: High blood pressure is a significant risk factor for both ischemic and hemorrhagic strokes.
- Atherosclerosis: The buildup of plaque in arteries can restrict blood flow.
- Diabetes: Increases the risk of vascular damage.
- Smoking: Contributes to arterial damage and increases clotting risk.
- Obesity: Linked to various cardiovascular conditions that elevate stroke risk.
- Sedentary Lifestyle: Lack of physical activity can contribute to obesity and other risk factors.
Other contributing factors may include genetic predispositions, atrial fibrillation (which increases stroke risk), and certain autoimmune disorders.
Symptoms and Clinical Presentation
The symptoms of cerebrovascular disease depend on the specific condition but may include:
- Sudden Weakness or Numbness: Typically affecting one side of the body (hemiparesis).
- Difficulty Speaking or Understanding Speech: Slurred speech or confusion.
- Vision Problems: Sudden loss or blurring of vision in one or both eyes.
- Severe Headache: Often described as a sudden “thunderclap” headache, particularly in hemorrhagic strokes.
- Loss of Balance or Coordination: Difficulty walking or maintaining balance.
Recognizing these symptoms promptly is critical for seeking emergency medical attention.
Diagnosis
Diagnosing cerebrovascular disease involves a combination of clinical evaluation and diagnostic imaging:
- Medical History Review: Gathering information about symptoms, risk factors, and family history.
- Physical Examination: Neurological assessments focusing on motor skills, reflexes, and cognitive function.
- Imaging Studies:
- CT Scan: Quickly identifies bleeding in cases of hemorrhagic stroke.
- MRI: Provides detailed images of brain tissue and can identify ischemic areas.
- Angiography: Visualizes blood vessels in the brain to detect blockages or malformations.
- Blood Tests: May be performed to assess cholesterol levels, clotting factors, and other relevant markers.
Treatment Options
Treatment for cerebrovascular disease varies based on the specific condition but generally aims to restore blood flow and manage symptoms:
- Medications:
- Anticoagulants: Such as warfarin or direct oral anticoagulants help prevent clot formation.
- Antiplatelet Agents: Aspirin or clopidogrel reduce the risk of future strokes by preventing platelet aggregation.
- Thrombolytics: Used in acute ischemic stroke cases to dissolve clots quickly.
- Surgical Interventions:
- Endarterectomy: Surgical removal of plaque from carotid arteries to improve blood flow.
- Angioplasty and Stenting: Minimally invasive procedures to open narrowed arteries using balloons and stents.
- Rehabilitation Services: Physical therapy, occupational therapy, and speech therapy may be necessary post-stroke to aid recovery.
Prognosis and Recovery
The prognosis for individuals with cerebrovascular disease depends on several factors:
- Type and Severity of Stroke: Ischemic strokes generally have better outcomes than hemorrhagic strokes.
- Timeliness of Treatment: Rapid intervention significantly improves recovery chances.
- Overall Health Status: Pre-existing conditions can impact recovery potential.
Many individuals experience varying degrees of recovery; however, some may face long-term disabilities requiring ongoing support.
Living with Cerebrovascular Disease
Living with cerebrovascular disease necessitates ongoing management:
- Regular Follow-ups: Continuous monitoring by healthcare providers is essential for managing long-term effects.
- Lifestyle Modifications: Adopting a heart-healthy diet, engaging in regular physical activity, quitting smoking, and managing stress are crucial for reducing stroke risk.
- Support Networks: Connecting with support groups provides emotional assistance for both patients and families navigating this condition.
Education about recognizing symptoms early empowers patients and caregivers to seek timely medical attention when needed.
Research and Future Directions
Research into cerebrovascular disease continues to advance our understanding of its mechanisms and treatment options:
- Neuroprotective Strategies: Investigating ways to protect brain tissue during ischemic events holds promise for improving outcomes.
- Innovative Therapies: New medications aimed at enhancing recovery after stroke are being explored.
These research efforts are crucial for improving patient care related to this complex condition.
Conclusion
Cerebrovascular disease represents a significant health challenge that requires prompt diagnosis and treatment. Understanding its causes, symptoms, diagnosis, treatment options, and long-term management strategies is essential for patients and caregivers alike. With ongoing research aimed at improving diagnosis and therapeutic options, there is hope for better outcomes for those affected by this challenging condition.
Disclaimer: This article is intended for informational purposes only and should not be considered medical advice. Always consult with a qualified healthcare provider regarding any medical concerns or conditions.