Encephalocele: Understanding, Managing, and Living with a Rare Birth Defect
Introduction
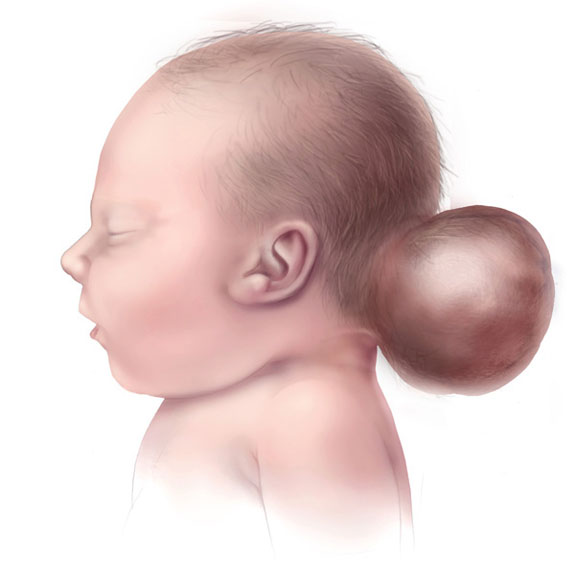
Encephalocele is a rare congenital condition characterized by the protrusion of brain tissue and its protective coverings through an opening in the skull. This defect can occur anywhere along the skull but is most commonly seen in the back of the head. The severity of encephalocele varies widely, ranging from small protrusions covered by skin to large sacs containing significant portions of brain tissue. Understanding the causes, symptoms, diagnosis, and treatment options for encephalocele is crucial for effective management and improving patient outcomes. This article provides a comprehensive overview of encephalocele, including its historical background, anatomy and pathophysiology, causes, symptoms and clinical presentation, diagnosis, treatment options, prognosis and recovery, living with encephalocele, research and future directions, and a conclusion summarizing key points.
What is an Encephalocele?
An encephalocele is defined as a neural tube defect where a portion of the brain and its protective membranes protrude through an abnormal opening in the skull. The condition occurs during fetal development when the neural tube does not close completely. Encephaloceles can be classified based on their location:
- Occipital Encephalocele: The most common type, located at the back of the head.
- Frontal Encephalocele: Located at the front of the head.
- Other Locations: Encephaloceles can also occur at various other sites along the skull.
The contents of an encephalocele may include brain tissue, cerebrospinal fluid (CSF), and membranes surrounding the brain.
Historical Background
The understanding of encephalocele has evolved significantly over time. Descriptions of cranial defects can be found in ancient medical texts; however, it wasn’t until the 20th century that encephaloceles began to be studied more systematically. Advances in imaging technology have allowed for earlier diagnosis during pregnancy through ultrasound examinations.In recent decades, increased awareness of neural tube defects has led to better understanding and management strategies for conditions like encephalocele. Research continues to focus on prevention and treatment options to improve outcomes for affected individuals.
Anatomy and Pathophysiology
To understand encephalocele fully, it is essential to examine normal brain anatomy:
- Normal Brain Structure: The brain is encased within the skull and protected by three layers of membranes called meninges. The skull serves as a barrier against injury.
- Pathophysiology: In encephalocele:
- A failure in neural tube closure during embryonic development results in an opening in the skull.
- Brain tissue may herniate through this opening, forming a sac-like structure.
- Depending on the size and contents of the sac, neurological function may be affected.
Understanding these anatomical changes helps clarify why individuals with encephalocele experience specific symptoms associated with this condition.
Causes
The exact causes of encephalocele are not fully understood; however, several risk factors have been identified:
- Genetic Factors: Certain genetic syndromes increase susceptibility to neural tube defects, including encephaloceles.
- Environmental Influences: Maternal exposure to certain environmental factors during pregnancy—such as medications (e.g., anticonvulsants), alcohol consumption, or nutritional deficiencies—may contribute to the development of encephaloceles.
- Folic Acid Deficiency: Insufficient intake of folic acid during pregnancy has been linked to an increased risk of neural tube defects.
Understanding these causes is crucial for developing effective prevention strategies against encephalocele.
Symptoms and Clinical Presentation
Symptoms associated with encephalocele can vary widely depending on its size and location but typically include:
- Visible Sac: A noticeable bulge or sac on the head that may be covered by skin or thin membranes.
- Neurological Symptoms: Depending on how much brain tissue is involved:
- Developmental delays.
- Seizures.
- Motor deficits or weakness.
- Hydrocephalus: Accumulation of cerebrospinal fluid within the brain may occur in some cases due to obstruction.
Symptoms may fluctuate based on individual health status and overall development.
Diagnosis
Diagnosing an encephalocele involves several steps:
- Medical History Review: A healthcare provider will inquire about family history and any prenatal exposures that may contribute to neural tube defects.
- Physical Examination: A thorough examination focuses on assessing visible signs such as bulging or deformities in the skull.
- Diagnostic Tests:
- Prenatal Ultrasound: Often used to detect encephaloceles during pregnancy; it can reveal abnormalities in fetal development.
- MRI (Magnetic Resonance Imaging): Provides detailed images of brain structures and can help assess associated anomalies after birth.
- CT Scan (Computed Tomography): May be used for further evaluation if needed.
Early diagnosis allows for timely intervention and effective management strategies tailored to individual needs.
Treatment Options
Treatment for encephalocele varies based on severity:
- Surgical Intervention:
- Surgery is typically required to repair the defect by removing the herniated tissue and closing the opening in the skull.
- The timing of surgery depends on factors such as the size of the sac and any associated complications like hydrocephalus.
- Management of Associated Conditions:
- If hydrocephalus is present, placement of a shunt may be necessary to drain excess cerebrospinal fluid.
- Ongoing monitoring for developmental delays or neurological issues post-surgery is essential.
A multidisciplinary approach involving pediatric neurosurgeons, neurologists, and rehabilitation specialists ensures comprehensive care for individuals with this condition.
Prognosis and Recovery
The prognosis for individuals diagnosed with encephalocele varies significantly based on several factors:
- Size and Location: Smaller sacs that do not contain functional brain tissue generally have better outcomes than larger sacs that do involve significant brain structures.
- Timeliness of Treatment: Early surgical intervention improves outcomes significantly; many patients experience substantial improvements following appropriate management.
Most patients can achieve satisfactory results through appropriate management; however, some individuals may continue experiencing challenges related to developmental delays or neurological issues even after treatment.
Living with Encephalocele
Living with an encephalocele presents unique challenges:
- Emotional Impact: The visible nature of this condition can lead to feelings of anxiety or depression. Support groups provide valuable resources for coping.
- Lifestyle Adjustments: Individuals should take preventive measures against infections—this includes practicing good hygiene and regular medical check-ups post-surgery.
- Education on Self-Care: Patients should learn how best to manage their condition—this includes recognizing early signs of complications related to their symptoms and understanding when it’s necessary to seek medical attention if symptoms worsen.
Encouraging open discussions about experiences related to living with an encephalocele fosters acceptance within communities while empowering affected individuals.
Research and Future Directions
Ongoing research into encephalocele focuses on several key areas:
- Genetic Studies: Investigating genetic predispositions will enhance understanding of susceptibility factors related to this congenital defect.
- Advancements in Treatment Modalities: Research into new surgical techniques aims at improving outcomes while minimizing complications associated with traditional treatments.
As knowledge about this condition expands through research efforts—there is hope for improved diagnostic methods along with enhanced treatment options leading toward better quality-of-life outcomes for those living with an encephalocele.
Conclusion
Encephalocele is a complex congenital condition that requires awareness and understanding among healthcare providers and patients alike. With advancements in medical science alongside increased awareness regarding this condition—there lies potential for improved outcomes allowing those affected by it—to lead fulfilling lives despite their challenges posed by significant health complications resulting from this disorder.
Disclaimer
This article is intended for informational purposes only and should not be considered medical advice. Always consult with a healthcare professional for diagnosis and treatment options tailored specifically towards individual circumstances.
