Endophthalmitis: A Comprehensive Guide to a Serious Eye Condition
Introduction
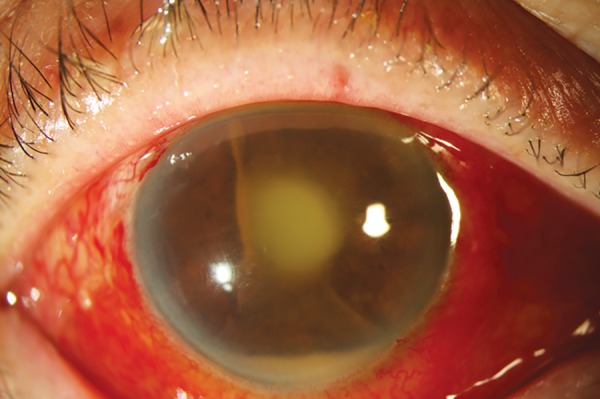
Endophthalmitis is a severe and potentially sight-threatening infection of the interior of the eye, characterized by inflammation of the vitreous and aqueous humor. This condition can lead to significant complications, including vision loss, if not diagnosed and treated promptly. Understanding endophthalmitis is crucial for both healthcare providers and patients, as early intervention can make a substantial difference in outcomes. This article will delve into the historical background, anatomy and pathophysiology, causes, symptoms and clinical presentation, diagnosis, treatment options, prognosis and recovery, living with endophthalmitis, current research, and future directions.
What is Endophthalmitis?
Endophthalmitis is defined as an inflammatory condition of the inner eye structures caused by infection. It can be classified into two main types:
- Exogenous Endophthalmitis: This type occurs due to external factors such as surgery (e.g., cataract surgery), trauma (e.g., penetrating eye injuries), or infections that enter through the eye’s surface.
- Endogenous Endophthalmitis: This type arises from infections that spread to the eye from other parts of the body through the bloodstream. Conditions like bacteremia or fungemia often lead to this form.
Both types require immediate medical attention to prevent irreversible damage to vision.
Historical Background
The understanding of endophthalmitis has evolved significantly over the years. The condition was first documented in the early 20th century when physicians began to recognize its association with surgical procedures. As surgical techniques improved, so did awareness of postoperative complications like endophthalmitis.In recent decades, advancements in microbiology and imaging technologies have enhanced our understanding of the pathogens responsible for endophthalmitis and how they invade ocular tissues. Studies have shown that bacteria such as Staphylococcus aureus and Streptococcus species are common culprits in exogenous cases, while fungi like Candida are often implicated in endogenous cases.
Anatomy and Pathophysiology
To fully understand endophthalmitis, it is essential to grasp the anatomy of the eye:
- Aqueous Humor: This clear fluid fills the front part of the eye (anterior chamber) and helps maintain intraocular pressure.
- Vitreous Humor: A gel-like substance that fills the larger posterior chamber of the eye.
In cases of endophthalmitis:
- Infection: Pathogens invade these fluids or tissues, leading to inflammation.
- Inflammatory Response: The body’s immune system responds by sending white blood cells to combat the infection, which can result in further tissue damage and vision impairment.
The presence of infection can lead to complications such as retinal detachment or permanent vision loss if not addressed promptly.
Causes
Several factors contribute to the development of endophthalmitis:
- Surgical Procedures: Eye surgeries such as cataract extraction or intraocular lens implantation can introduce bacteria into the eye.
- Trauma: Penetrating injuries can allow pathogens to enter directly.
- Systemic Infections: Conditions such as sepsis or infections from dental procedures can lead to endogenous endophthalmitis when bacteria travel through the bloodstream.
- Intravitreal Injections: Increasingly common treatments for various ocular conditions may inadvertently introduce pathogens into the eye.
Understanding these causes is vital for prevention strategies and early intervention.
Symptoms and Clinical Presentation
Symptoms of endophthalmitis can vary but commonly include:
- Severe Eye Pain: Often described as sharp or throbbing pain.
- Redness: Noticeable redness in the white part of the eye (sclera).
- Decreased Vision: Sudden loss or blurring of vision.
- Sensitivity to Light: Increased discomfort when exposed to bright lights (photophobia).
- Swelling of Eyelids: In some cases, eyelid swelling may occur.
These symptoms may develop rapidly, making it critical for individuals experiencing them to seek immediate medical attention.
Diagnosis
Diagnosing endophthalmitis typically involves several steps:
- Medical History Review: A thorough history including recent surgeries, trauma, or systemic infections.
- Ocular Examination: An ophthalmologist will conduct a comprehensive examination using tools such as slit-lamp microscopy.
- Cultures:
- Samples from aqueous humor and vitreous humor are taken for laboratory analysis to identify causative organisms.
- Blood cultures may also be performed if endogenous endophthalmitis is suspected.
Early diagnosis is critical for effective management and reducing risks associated with untreated endophthalmitis.
Treatment Options
Treatment for endophthalmitis is urgent and multifaceted:
- Antibiotic Therapy:
- Intravitreal antibiotics are administered directly into the eye; common choices include vancomycin combined with ceftazidime or amikacin.
- Systemic antibiotics may also be used depending on the severity and type of infection.
- Corticosteroids:
- Corticosteroids may be administered either systemically or intravitreally to reduce inflammation.
- Surgical Intervention:
- Vitrectomy: This surgical procedure involves removing infected vitreous gel from inside the eye. It is often necessary for severe cases where vision is threatened.
- Drainage procedures may also be performed if abscesses are present.
Prompt treatment is essential; delays can result in irreversible vision loss.
Prognosis and Recovery
The prognosis for individuals with endophthalmitis varies based on several factors:
- Timeliness of Treatment: Early intervention significantly improves outcomes; most patients respond well when treated promptly.
- Severity of Infection: The extent of damage at presentation plays a crucial role in recovery. Patients with severe vision loss at initial presentation may have poorer outcomes even with treatment.
After successful treatment, many individuals can expect some degree of visual recovery; however, ongoing monitoring remains crucial due to potential recurrence or complications.
Living with Endophthalmitis
Living with a history of endophthalmitis requires proactive health management:
- Regular Check-ups: Individuals should maintain regular appointments with their ophthalmologist for monitoring.
- Lifestyle Modifications:
- Protecting eyes from injury
- Managing underlying health conditions that could predispose them to infections
Emotional support from friends or support groups can also be beneficial as individuals navigate their diagnosis and treatment options.
Research and Future Directions
Current research efforts focus on improving understanding and management strategies for endophthalmitis:
- Innovative Treatments: Ongoing studies explore new antibiotic regimens that could provide more effective management with fewer side effects.
- Genetic Studies: Investigating genetic predispositions could lead to better prevention strategies for at-risk populations.
Continued research will enhance clinical practices surrounding this condition while improving patient outcomes in future years.
Conclusion
Endophthalmitis is a serious condition that requires immediate attention due to its potential implications for vision health. With advancements in diagnostic techniques and treatment modalities available today, many individuals can manage this condition effectively. Increased awareness among healthcare providers about risk factors, types of endophthalmitis, and appropriate management strategies is essential for improving patient care in this area.
Disclaimer: This article is intended for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for diagnosis and treatment options.