Eosinophilic Esophagitis: Understanding a Complex Esophageal Condition
Introduction
Eosinophilic Esophagitis (EoE) is an increasingly recognized chronic inflammatory condition of the esophagus characterized by an elevated number of eosinophils, a type of white blood cell. This condition affects both children and adults, leading to significant discomfort and complications if left untreated. As awareness of EoE grows, so does the need for comprehensive information on its causes, symptoms, diagnosis, treatment options, and ongoing research. This article aims to provide a detailed overview of Eosinophilic Esophagitis, helping patients and healthcare providers better understand this complex disorder.
What is Eosinophilic Esophagitis?
Eosinophilic Esophagitis is defined as an immune-mediated condition in which eosinophils accumulate in the esophageal tissue. This accumulation can lead to inflammation, resulting in esophageal dysfunction. The diagnosis of EoE requires the presence of at least 15 eosinophils per high-power field in esophageal biopsies, along with symptoms consistent with esophageal dysfunction.Patients with EoE often experience difficulty swallowing (dysphagia), food impaction, and chest pain that is not related to heart issues. The condition is distinct from gastroesophageal reflux disease (GERD), although some symptoms may overlap. Understanding the nuances of EoE is essential for effective management and treatment.
Historical Background
The recognition of Eosinophilic Esophagitis has evolved significantly over the past few decades. Initially described in the 1970s, EoE was often misdiagnosed or overlooked due to its similarity to other gastrointestinal disorders. It wasn’t until the late 1990s that the medical community began to identify EoE as a distinct clinical entity.Research has shown that EoE is becoming increasingly prevalent, particularly among children and young adults. The rise in diagnoses has been attributed to greater awareness among healthcare providers and advancements in diagnostic techniques such as endoscopy and biopsy.
Anatomy and Pathophysiology
To understand Eosinophilic Esophagitis better, it is essential to explore its anatomy and pathophysiology:
- Esophagus: The esophagus is a muscular tube connecting the throat to the stomach. It plays a crucial role in transporting food and liquids from the mouth to the stomach.
- Eosinophils: These white blood cells are part of the immune system and are primarily involved in combating parasitic infections and mediating allergic reactions. In EoE, eosinophils infiltrate the esophageal tissue, leading to inflammation and damage.
- Inflammatory Response: The presence of eosinophils triggers an inflammatory response that can result in tissue remodeling, fibrosis, and strictures over time if left untreated. This remodeling can lead to narrowing of the esophagus, making it difficult for food to pass through.
Understanding these biological mechanisms is crucial for diagnosing and managing EoE effectively.
Causes
The exact cause of Eosinophilic Esophagitis remains unclear; however, several factors have been identified as potential contributors:
- Allergic Reactions: Many patients with EoE have a history of atopic conditions such as asthma, allergic rhinitis, or eczema. Food allergies are particularly common triggers for eosinophil accumulation in the esophagus.
- Environmental Factors: Exposure to environmental allergens may play a role in triggering EoE symptoms. Increased pollution and dietary changes may also contribute to rising rates of this condition.
- Genetic Predisposition: Some individuals may have a genetic predisposition that makes them more susceptible to developing EoE when exposed to certain allergens or environmental factors.
- Gastrointestinal Microbiome: Emerging research suggests that alterations in gut microbiota may influence immune responses related to EoE.
Identifying these causes is essential for preventing further cases of EoE and managing existing conditions effectively.
Symptoms and Clinical Presentation
The symptoms of Eosinophilic Esophagitis can vary widely among individuals but typically include:
- Dysphagia: Difficulty swallowing solid foods or liquids.
- Food Impaction: Food becoming lodged in the esophagus, often requiring medical intervention.
- Chest Pain: Pain that mimics heart-related issues but is related to esophageal dysfunction.
- Nausea or Vomiting: Some patients may experience gastrointestinal distress.
- Weight Loss: In severe cases where eating becomes difficult.
- Heartburn or Acid Reflux Symptoms: Although distinct from GERD, some patients may report similar symptoms.
These symptoms can significantly impact daily functioning and quality of life.
Diagnosis
Diagnosing Eosinophilic Esophagitis involves several steps:
- Clinical Evaluation: A thorough medical history and physical examination are essential for identifying symptoms consistent with EoE.
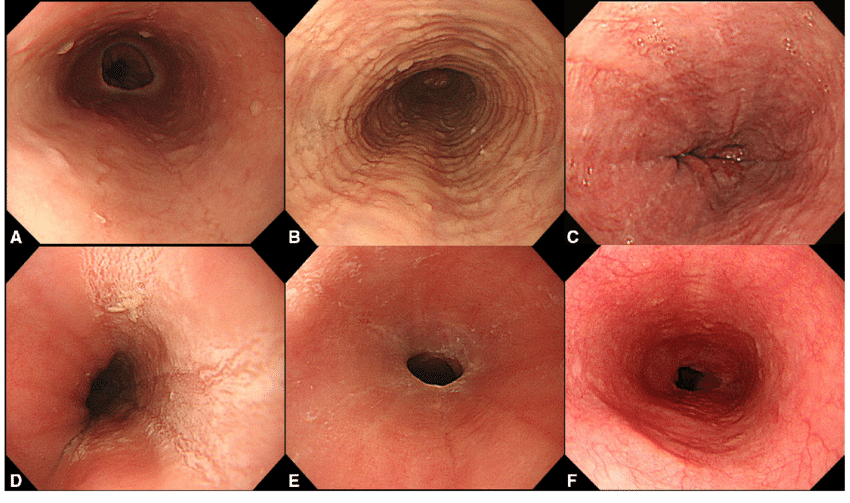
- Upper Endoscopy: An upper endoscopy allows direct visualization of the esophagus and enables biopsy collection from multiple sites along the esophagus to assess eosinophil levels.
- Biopsy Analysis: Histological examination of biopsies will reveal eosinophil counts greater than 15 per high-power field, confirming a diagnosis of EoE.
- Exclusion of Other Conditions: It is crucial to rule out other potential causes of eosinophilia or esophageal dysfunction such as GERD or infections before confirming a diagnosis of EoE.
- Allergy Testing: In some cases, allergy testing may be performed to identify specific food triggers associated with symptoms.
A comprehensive diagnostic approach ensures accurate identification of EoE.
Treatment Options
Treatment for Eosinophilic Esophagitis primarily focuses on managing symptoms and addressing underlying causes:
- Dietary Management:
- Elimination Diets: Removing common allergens such as dairy, wheat, soy, eggs, and nuts from the diet can help reduce inflammation.
- Elemental Diets: In severe cases where multiple food allergies are suspected, an elemental diet consisting solely of amino acid-based formulas may be necessary.
- Medications:
- Proton Pump Inhibitors (PPIs): These medications reduce stomach acid production and have been shown to improve symptoms in some patients with EoE.
- Topical Corticosteroids: Swallowed corticosteroids like budesonide can help reduce inflammation directly within the esophagus.
- Biologics: Medications such as Dupixent (dupilumab) have recently been approved for treating moderate-to-severe cases of EoE by targeting specific inflammatory pathways.
- Esophageal Dilation: In cases where strictures develop due to chronic inflammation, endoscopic dilation may be performed to widen the esophagus.
- Ongoing Monitoring: Regular follow-ups with healthcare providers are essential for assessing treatment effectiveness and making necessary adjustments.
Each treatment plan should be individualized based on patient needs and specific circumstances.
Prognosis and Recovery
The prognosis for individuals with Eosinophilic Esophagitis varies widely based on several factors:
- Severity of Symptoms: Patients with milder forms of EoE often experience better outcomes compared to those with severe complications.
- Timeliness of Treatment: Early diagnosis and intervention play a crucial role in improving recovery rates.
- Long-Term Monitoring: Patients require ongoing monitoring for potential complications such as strictures or persistent dysphagia.
Overall, while many patients can achieve significant symptom relief with appropriate management strategies, some may experience chronic symptoms requiring continuous care.
Living with Eosinophilic Esophagitis
Living with Eosinophilic Esophagitis can be challenging but manageable with appropriate strategies:
- Education: Understanding triggers empowers patients to recognize situations that exacerbate symptoms.
- Lifestyle Adjustments:
- Maintaining a healthy diet tailored to individual needs can support overall well-being.
- Regular exercise tailored to individual capabilities can improve physical function.
- Support Networks: Connecting with support groups provides emotional assistance from others facing similar challenges.
- Regular Medical Care: Ongoing consultations with healthcare providers ensure timely adjustments to treatment plans based on evolving needs.
By adopting proactive measures, individuals can enhance their quality of life despite living with this condition.
Research and Future Directions
Ongoing research continues to explore various aspects of Eosinophilic Esophagitis:
- Mechanisms of Disease: Investigating how specific allergens trigger eosinophilic responses could lead to better preventive measures.
- Genetic Studies: Understanding genetic predispositions may help identify individuals at risk for developing EoE after exposure to dietary allergens.
- Novel Treatments: Research into targeted therapies could improve outcomes for patients suffering from severe manifestations of EoE.
- Public Health Initiatives: Increasing awareness about food allergies will help prevent future cases linked to dietary triggers associated with this condition.
These advancements hold promise for improving prevention strategies and treatment options for those affected by Eosinophilic Esophagitis.
Conclusion
Eosinophilic Esophagitis is a complex condition that requires comprehensive understanding for effective management. By recognizing triggers, utilizing effective treatments, and staying informed about ongoing research developments, individuals can navigate their health challenges more effectively. As our understanding evolves, there is hope for improved outcomes for those affected by this increasingly prevalent disorder.
Disclaimer
This article is intended for informational purposes only and should not be considered medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment options tailored to your specific situation.
