Thyroid Eye Disease: Understanding, Diagnosis, and Treatment Options
Introduction
Thyroid eye disease (TED), also known as Graves’ ophthalmopathy or Graves’ disease, is an autoimmune condition that affects the eyes and is commonly associated with thyroid dysfunction. This condition can significantly impact a person’s quality of life due to its physical and psychological effects. Understanding thyroid eye disease is essential for early diagnosis and effective management. This article aims to provide a comprehensive overview of TED, including its causes, symptoms, diagnosis, treatment options, and ongoing research.
What Is Thyroid Eye Disease?
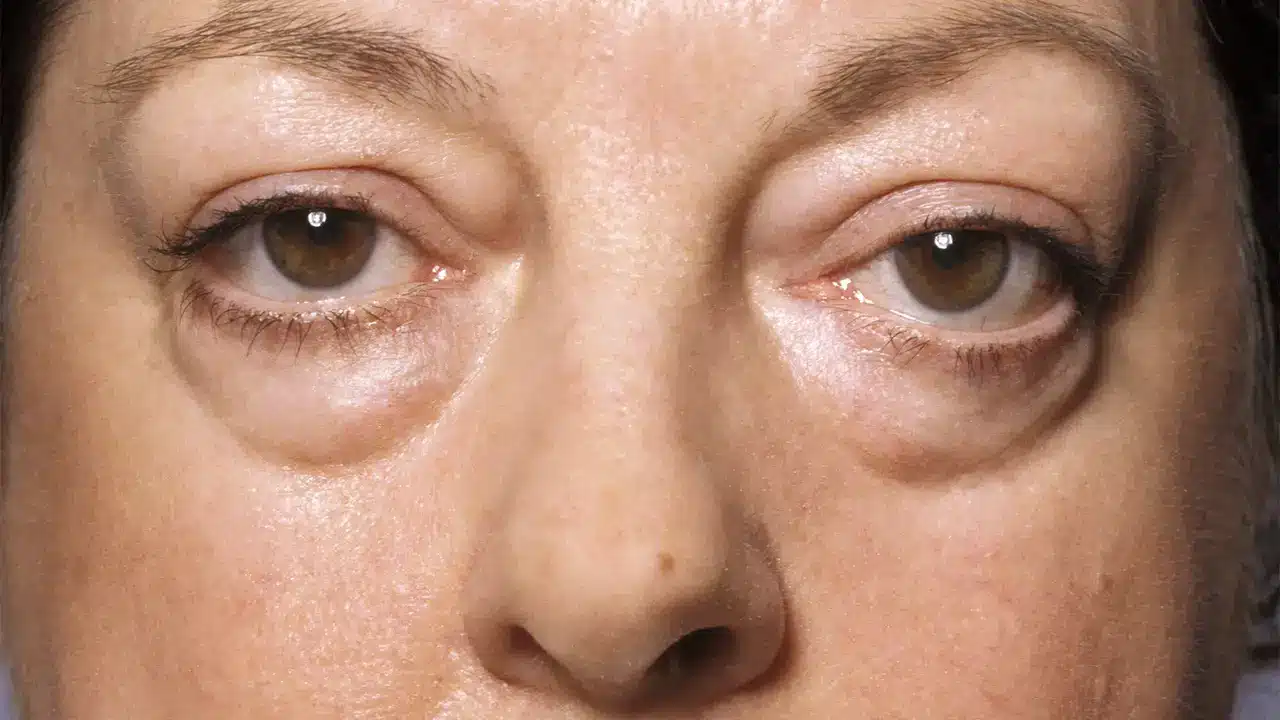
Thyroid eye disease is an autoimmune disorder in which the body’s immune system mistakenly attacks the tissues surrounding the eyes. This leads to inflammation and swelling of the eye muscles, fat, and connective tissue behind the eyes. TED is most often associated with hyperthyroidism caused by Graves’ disease but can also occur in individuals with normal or low thyroid hormone levels. Symptoms may include bulging eyes (proptosis), double vision, dry eyes, and eyelid retraction.
Historical Background
The understanding of thyroid eye disease has evolved over time. Historically, symptoms such as bulging eyes were often attributed to various causes without a clear connection to thyroid function. In the early 20th century, researchers began to recognize the link between Graves’ disease and eye symptoms. As medical knowledge advanced, TED was identified as a distinct condition requiring specific diagnostic criteria and treatment approaches.
Anatomy and Pathophysiology
The thyroid gland is located at the base of the neck and produces hormones that regulate metabolism. In thyroid eye disease, the immune system attacks not only the thyroid gland but also the tissues around the eyes. The inflammation leads to swelling of the extraocular muscles and fat behind the eyes. This swelling can push the eyes forward, causing proptosis (bulging) and restricting eye movement, which may result in double vision.
Causes
The primary cause of thyroid eye disease is an autoimmune response triggered by factors such as:
- Graves’ Disease: The most common cause of TED; it results in overproduction of thyroid hormones due to antibodies attacking the thyroid gland.
- Genetic Factors: A family history of autoimmune diseases may increase susceptibility.
- Environmental Triggers: Smoking is a significant risk factor; smokers are two to eight times more likely to develop TED.
- Hormonal Changes: Fluctuations in hormone levels can exacerbate symptoms.
Symptoms and Clinical Presentation
Symptoms of thyroid eye disease can vary in severity and may include:
- Proptosis: Bulging or protrusion of one or both eyes.
- Eyelid Retraction: The upper eyelid may appear elevated.
- Double Vision: Caused by misalignment of the eyes.
- Dryness or Grittiness: A sensation of having sand in the eyes due to exposure.
- Redness or Swelling: Inflammation may lead to redness in the whites of the eyes (sclera).
- Pain or Discomfort: Pain behind the eyes or during eye movement may occur.
Symptoms often develop gradually over several months but can worsen within the first year after diagnosis.
Diagnosis
Diagnosing thyroid eye disease involves several steps:
- Medical History: A thorough review of symptoms and any history of thyroid disorders.
- Physical Examination: An ophthalmologist will assess eye movement, appearance, and any signs of inflammation.
- Blood Tests: These tests measure levels of thyroid hormones (T3, T4) and Thyroid Stimulating Hormone (TSH) to evaluate thyroid function.
- Imaging Studies: CT scans or MRIs may be used to visualize changes in the orbit (eye socket) and assess muscle involvement.
Treatment Options
Treatment for thyroid eye disease varies based on severity:
Mild Cases
- Artificial Tears: Over-the-counter lubricating eye drops help relieve dryness.
- Selenium Supplements: Some studies suggest that selenium may reduce inflammation.
Moderate to Severe Cases
- Corticosteroids: Medications like prednisone can help reduce inflammation.
- Teprotumumab (Tepezza): A newer medication specifically approved for treating TED that targets underlying processes causing inflammation.
- Orbital Radiotherapy: This treatment uses targeted radiation to reduce inflammation around the eyes.
Surgical Options
In cases where vision is threatened or cosmetic concerns arise:
- Decompression Surgery: Removes bone from around the orbit to relieve pressure on the optic nerve.
- Eye Muscle Surgery: Corrects misalignment caused by enlarged muscles.
- Eyelid Surgery: Addresses eyelid retraction or cosmetic concerns related to proptosis.
Prognosis and Recovery
The prognosis for individuals with thyroid eye disease varies based on severity and response to treatment:
- Mild cases often improve over time without intervention.
- Moderate to severe cases may require ongoing management; early treatment can prevent complications such as vision loss.
Recovery timelines depend on treatment type; surgical recovery typically takes several weeks while ongoing monitoring is essential for all patients.
Living with Thyroid Eye Disease
Managing life with thyroid eye disease involves several considerations:
- Regular Monitoring: Consistent follow-up appointments are crucial for managing symptoms effectively.
- Support Systems: Engaging with support groups can provide emotional support and practical advice from others facing similar challenges.
- Lifestyle Changes: Quitting smoking can significantly improve outcomes; maintaining a healthy diet and regular exercise can also support overall well-being.
Research and Future Directions
Ongoing research into thyroid eye disease focuses on understanding its underlying mechanisms better and identifying new therapeutic targets. Studies are exploring links between lifestyle factors (such as diet) and disease development while investigating novel treatments that target specific pathways involved in inflammation.
Conclusion
Thyroid eye disease is a complex condition that requires awareness for effective management. Understanding its causes, symptoms, diagnosis methods, treatment options, and lifestyle adjustments can empower individuals facing this condition. If you experience persistent symptoms or have concerns about your health, seeking medical advice is crucial for appropriate care.
Disclaimer
This article is intended for informational purposes only and should not be considered medical advice. Always consult a healthcare professional for diagnosis and treatment options tailored to your specific needs.
