Tendonitis: Causes, Symptoms, and Treatment Options
Introduction
Tendonitis, also known as tendinitis, is a common condition characterized by the inflammation or irritation of a tendon, the thick fibrous cords that connect muscles to bones. This condition can cause significant pain and discomfort, limiting mobility and affecting daily activities. Understanding tendonitis is crucial for recognizing its symptoms, identifying potential causes, and exploring effective treatment options. This article will provide a comprehensive overview of tendonitis, including its historical background, anatomy, causes, symptoms, diagnosis, treatment options, and ongoing research.
What Is Tendonitis?
Tendonitis refers to the inflammation of a tendon due to overuse or injury. It can occur in any tendon in the body but is most commonly seen in areas such as the shoulders, elbows, knees, and Achilles tendon. The inflammation can lead to pain, swelling, and reduced function in the affected area.
Characteristics of Tendonitis
- Localized Pain: Pain is typically felt at the site of the affected tendon and may worsen with movement.
- Swelling: The area around the tendon may appear swollen or thickened.
- Reduced Range of Motion: Individuals may experience stiffness or difficulty moving the affected joint.
- Tenderness: The tendon may be sensitive to touch or pressure.
Historical Background
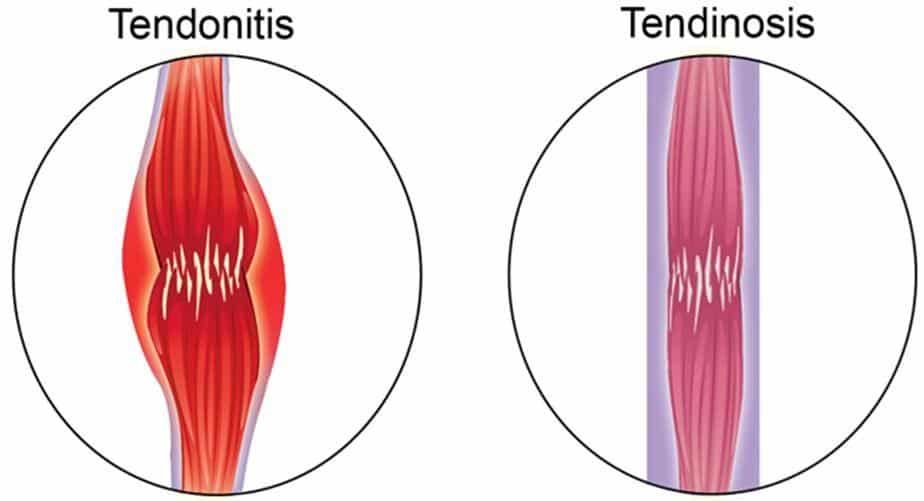
The understanding of tendonitis has evolved significantly over time. Early descriptions of tendon injuries date back to ancient civilizations; however, it wasn’t until the 19th century that specific conditions related to tendons began to be formally recognized. Initially grouped under general inflammatory conditions, tendonitis gained attention as researchers identified distinct patterns associated with repetitive strain injuries. As medical knowledge advanced in the late 20th century, tendonitis was differentiated from other forms of tendon injuries like tendinosis, leading to more effective treatment strategies.
Anatomy and Pathophysiology
To understand tendonitis better, it is important to consider the anatomy involved:
Key Structures
- Tendons: Tendons are strong bands of connective tissue that attach muscles to bones. They are primarily composed of collagen fibers arranged in parallel bundles.
- Muscles: Muscles contract to produce movement and exert force on tendons.
- Joints: Tendons cross joints to facilitate movement; therefore, any dysfunction can impact joint function.
Pathophysiology
The pathophysiology of tendonitis involves several key processes:
- Microtrauma: Repetitive stress on a tendon leads to microtears in collagen fibers.
- Inflammatory Response: Inflammatory cells migrate to the site of injury, causing swelling and pain.
- Degenerative Changes: Over time, chronic inflammation can lead to degenerative changes in the tendon structure.
These physiological changes contribute to the development of symptoms associated with tendonitis.
Causes
Several factors can contribute to the development of tendonitis:
Overuse Injuries
- Repetitive Activities: Engaging in repetitive motions or activities that strain a tendon can lead to microtrauma over time.
- Sudden Increases in Activity: Rapidly increasing the intensity or duration of physical activity can overwhelm tendons.
Anatomical Factors
- Biomechanical Issues: Abnormalities in foot structure or alignment can place excessive stress on certain tendons.
- Muscle Imbalances: Weakness or tightness in surrounding muscles can affect how forces are distributed across a tendon.
Age-related Changes
- Degenerative Changes: As individuals age, tendons naturally lose elasticity and strength, making them more susceptible to injury.
Other Contributing Factors
- Poor Technique: Improper technique during sports or physical activities can increase the risk of developing tendonitis.
- Medical Conditions: Conditions such as diabetes or rheumatoid arthritis can predispose individuals to tendon injuries.
Understanding these causes helps identify individuals at risk for developing tendonitis.
Symptoms and Clinical Presentation
Symptoms of tendonitis can vary based on the specific tendon affected but commonly include:
General Symptoms
- Localized Pain: Pain at the site of the tendon that worsens with activity.
- Swelling: There may be visible swelling or thickening around the affected area.
- Stiffness: Reduced range of motion or stiffness after periods of inactivity.
Specific Symptoms by Location
- Achilles Tendonitis:
- Pain along the back of the ankle or heel.
- Stiffness in the morning that improves with activity.
- Patellar Tendonitis (Jumper’s Knee):
- Pain at the front of the knee during jumping or running activities.
- Tenderness below the kneecap.
- Rotator Cuff Tendonitis:
- Shoulder pain that worsens with overhead activities.
- Weakness when lifting objects.
- Tennis Elbow (Lateral Epicondylitis):
- Pain on the outer part of the elbow that radiates down the forearm.
- Discomfort when gripping or lifting objects.
Recognizing these symptoms early is crucial for timely diagnosis and intervention.
Diagnosis
Diagnosing tendonitis involves several steps:
- Medical History Review: A healthcare provider will assess symptoms and any previous injuries related to the affected tendon.
- Physical Examination: A thorough examination will evaluate tenderness, swelling, range of motion, and strength in the affected area.
- Imaging Studies:
- X-rays: Initial imaging may reveal any bony abnormalities or calcifications around tendons.
- Ultrasound: This imaging technique can visualize soft tissues and assess for tears or degeneration in tendons.
- MRI (Magnetic Resonance Imaging): Provides detailed images of soft tissues and helps evaluate more complex cases.
An accurate diagnosis allows for tailored treatment strategies.
Treatment Options
Treatment for tendonitis focuses on reducing pain and improving function:
Medical Treatments
- Rest and Activity Modification:
- Avoiding activities that exacerbate symptoms is crucial for recovery.
- Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen may help alleviate pain and inflammation.
- Corticosteroid injections may be considered for severe inflammation but should be used judiciously due to potential side effects.
- Physical Therapy:
- Physical therapy plays a vital role in rehabilitation by focusing on stretching exercises, strengthening exercises, and improving biomechanics.
- Surgical Options:
- In severe cases where conservative treatments fail after several months, surgical intervention may be considered to repair damaged tissue or remove degenerated tissue.
Home Remedies and Lifestyle Interventions
Individuals can adopt several strategies at home:
- Ice Therapy: Applying ice packs can help reduce swelling and alleviate pain after activity.
- Compression Wraps: Using elastic bandages can help minimize swelling during recovery.
- Gentle Stretching Exercises: Engaging in gentle stretching routines may improve flexibility without exacerbating symptoms.
Prognosis and Recovery
The prognosis for individuals with tendonitis varies based on several factors:
- Severity of Symptoms: Many individuals experience significant improvement with appropriate treatment; however, some may continue to have chronic symptoms despite intervention.
Recovery timelines differ; some individuals may see improvements within weeks while others may require ongoing management for months.
Living with Tendonitis
Managing life with tendonitis involves ongoing care strategies:
- Regular Follow-ups: Routine visits with healthcare providers are essential for monitoring progress after treatment.
- Education About Condition: Understanding your specific type of tendonitis empowers you to make informed decisions about your healthcare options.
- Support Networks: Connecting with support groups can provide valuable resources and emotional support during challenging times.
Research and Future Directions
Ongoing research into tendonitis aims to enhance understanding of its etiology and improve treatment outcomes. Areas of focus include:
- Investigating genetic factors that might influence susceptibility to developing this condition.
- Exploring new treatment modalities such as regenerative medicine techniques like platelet-rich plasma (PRP) therapy or stem cell therapy.
These advancements hold promise for improving outcomes for individuals affected by this condition.
Conclusion
Tendonitis is a common yet often distressing condition that requires careful management and understanding. By recognizing its causes, symptoms, diagnostic methods, and treatment options, those affected by this condition can take proactive steps toward better health outcomes. If you suspect you have symptoms related to tendonitis or have concerns about your health status, consult a healthcare professional for personalized advice.
Disclaimer
This article is intended for informational purposes only and should not be considered medical advice. Always consult a qualified healthcare provider for diagnosis and treatment tailored to your individual needs.
